Walking Again With the Help of Technology
15 Sep 2019Sixty-six-year-old Mdm Hee did not appear a likely candidate for stroke. An active and independent senior, she held a job and did household chores herself. It came as a complete surprise to her when she had a stroke in November 2018.
“I remember it was a Monday. I had my lunch and sat down to watch television. My face began to itch, and I felt like I was floating when I was walking,” she recalled. “I took a bath thinking it would help, but it didn’t. Slowly, I began to feel worse as the day went on. So my family called for an ambulance.”
By the Lunar New Year of 2019, a clot the size of a coin was discovered in her brain. Fearing that it could rupture anytime, Mdm Hee was operated on immediately.
“After the surgery I experienced weakness on my left side and I couldn’t lift my left leg up at all,” she said. Determined to regain her active lifestyle again, Mdm Hee chose to stay in the hospital to complete her rehabilitation. “I want to go back to work,” she said.
Post-stroke rehabilitation
Not every stroke patient is as eager for rehabilitation as Mdm Hee. A local study published in 2014 found that only one in five stroke patients who are discharged from the hospital continue with their rehabilitation programme just three months after discharge from the hospital*. And by the end of the year, only one in 20 would continue.
Many patients find the rehabilitation process daunting, especially the elderly. The lack of physical mobility, not having anyone to bring them for rehabilitation sessions and the long recovery process are some of the difficulties faced.
Without rehabilitation, patients’ physical abilities deteriorate, and they may become more frail.
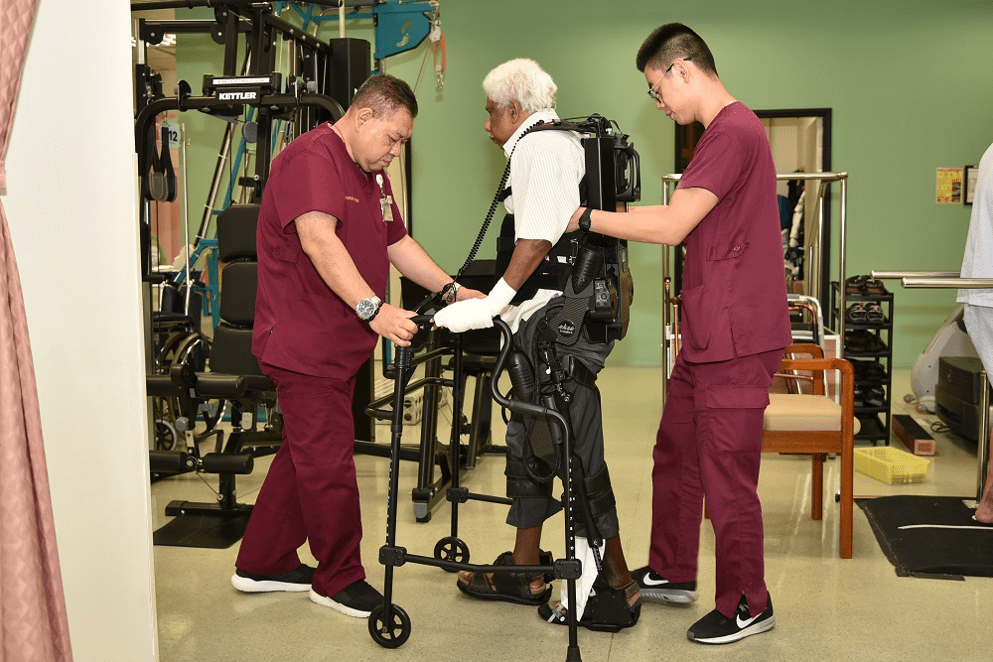
Piloting the use of exoskeleton technology in community-based rehabilitation for seniors
To improve the rehabilitation outcomes of seniors with physical disabilities, a new pilot programme is bringing bionic exoskeleton technology into the community. Funded by the Balaji Sadasivan Endowment managed by Temasek Foundation, the Temasek Foundation – Improving Mobility via Exoskeletons (iMOVE) programme is piloted at five different rehabilitation settings:
- A transitional rehabilitation ward run by National University Hospital (NUH) at the Alexandra campus;
- A community-based inpatient and day rehabilitation centre by St Luke’s Hospital;
- A nursing home under NTUC Health;
- A senior care centre under St. Luke’s Eldercare, and
- A community-based stroke support and Activity Group by Stroke Support Station.
Benefits of therapy with bionic exoskeleton
An exoskeleton robotic device is a wearable robotic device which is designed to help patients with disabilities or weakness result from a spinal cord injury, stroke or other conditions. Programmed to mimic normal walking patterns, therapists can help their patients to stand upright, walk and turn assisted by the device. Patients can re-learn step patterns and weight shifting, with the aim of regaining as much of their natural gait as possible.

Mr Ong Zhong Li, a physiotherapist at Alexandra Hospital explained how he employs the bionic exoskeleton in a physiotherapy session. “We start them (the patients) off by standing up, and get them to find their midline, to get them balanced. The exoskeleton can provide some assistance. Once the patient is accustomed to the system and the way the exoskeleton walks, we can put them on free legs and get them to walk. And if they are better we can give them resistance, to challenge them to work even harder.”
The exoskeleton improves patient recovery over a shorter period of rehabilitation, making it a more cost- and manpower-efficient therapy treatment. As part of the pilot programme, NUH has brought in two types of exoskeletons to determine their suitability for the local population across different health conditions and rehabilitation settings. Dr Effie Chew, Chief of Rehabilitation Services at Alexandra Hospital and a senior consultant in Rehabilitation Medicine, Department of Neurology, NUH, is leading the study which hopes to recruit 400 patients. “With this study, we hope to give patients the best chances of achieving their fullest potential in recovery with the help of the latest in rehabilitation technology. We have had good initial experience with the technology, with better and faster improvement in mobility for some of our patients and hope to see the benefits brought to more patients in the community.”
“We have become hopeful”
For those who have been by the side of their loved ones coping with stroke, rehabilitation therapy with exoskeleton has brought some cautious optimism.

Mdm Letchmi is a nurse with 30 years of experience at a local hospital, and the main caregiver of her husband, Mr Gandhi, who has a spinal cord injury and not been able to walk for two years following an operation. Seeing her once-active husband confined to his bed has been tough. “He is in pain even when he is asleep. It’s difficult for him, from being active to becoming like this,” she said.
Like Mdm Hee, Mr Gandhi was one of the first in Singapore to use exoskeleton as part of his rehabilitation. “At his first session, he could move a bit, and felt lighter. So there is motivation for him to continue,” said Mdm Letchmi.
Mr Gandhi has since completed 15 sessions using exoskeleton. “He is slowly improving – he can stand for a short time. There is a little bit of progress; it’s still early to say, because it’s only been two months. But we have become hopeful.”